THE NEXT PANDEMIC

By the time the general populace paid attention to the emergence and spread of SARS-CoV-2, and before businesses closed, “COVID-19” and “coronavirus” entered everyday conversations, and students in grades K-college were suddenly homeschoolers, Bart Tarbet, Brett Hurst, and other researchers around the world had already invested weeks of work trying to understand and defeat the novel coronavirus.
Although war metaphors abound in the near-constant news about the world’s response to this particular coronavirus, “defeat” may not be the word to describe the researchers’ objectives. People talk about fighting or battling the virus, but SARS-CoV-2 didn’t declare war on us. The virus just is and it does what viruses do: get into the cells of a host and replicate itself. Humans may have moved on from feeling anxious and frightened to bored with the virus, but the virus doesn’t care and it’s not going away.
“We have learned a lot in a very short time but we still have work to do to develop a successful treatment or vaccine,” Hurst, a research assistant professor in USU’s College of Agriculture and Applied Sciences, says. “We don’t have a miracle cure or way to prevent the spread of this virus, so we are doing the same things that we have done for months—social distancing, wearing masks, and increased hygiene procedures. Many of us have grown tired of the repetitive nature of these tasks and the limitations on our activities so we become more lax in our approach. Our social patience has worn out even though the virus is still spreading.”

SARS-CoV-2, also known as COVID-19, is the fifth major emerging disease USU researcher Bart Tarbet has studied. Photo by Levi Sim.
Tarbet, a USU research associate professor, says every pandemic or major disease outbreak has two endings—one social and one medical. He calculates that since he started graduate school in 1992, gained 12 years of experience in commercial vaccine development, and joined USU’s Institute for Antiviral Research (IAR) in 2008, SARS-CoV-2 is the fifth major emerging disease he has worked on and watched play out socially and medically. He and his colleagues have repeatedly seen that the two pandemic “endings” do not coincide because people are always ready to move on or get back to normal well before the virus threat has passed.
So while people around the world feel like many facets of life have been put on pause, work at the IAR and other labs around the world continues at an accelerated pace. But working with this virus requires methodical attention to detail and incubation times don’t speed up just because researchers feel a heightened sense of urgency.
“In the past 30 years, 70 percent of new and emerging diseases in humans have come from animals. And 50 percent of physicians could not diagnose a zoonotic illness because it’s an animal disease.” – Bart Tarbet
Tarbet, Hurst, and technicians who work with them, with funding from the National Institutes of Health, are testing the effects of several antiviral compounds used to treat or prevent other viral diseases on the novel coronavirus. The team also tests drugs and vaccines for pharmaceutical companies. The institute has a number of coronaviruses—SARS, MERS, what they call seasonal coronaviruses, and SARS-CoV2—and have evaluated several drugs against them. Some are promising and many are not.
In addition to tests in Petri dishes and test tubes, the researchers may use animal models after a drug appears effective through in vitro testing. Among the important animal models they use are golden Syrian hamsters that are genetically engineered to be susceptible to some diseases that occur in humans. Professor Zhongde Wang in USU’s Department of Animal, Dairy and Veterinary Sciences engineered the transgenic hamsters being used in COVID-19 model development. Tarbet points out that testing can’t be rushed and in vivo testing is a hurdle that many drugs and antiviral compounds fail to clear. It is also a mandatory step on the path to U.S. Food and Drug Administration approval of a new drug or a new use for an existing one.
At USU, studies with serious biohazards like SARS-CoV2 are done in the IAR’s biosafety level (BSL)3 and BSL3+ laboratories. The labs have elaborate airflow systems, containment equipment, and anterooms where the scientists change into and out of personal protective equipment. There is no place for a cell phone or anything else that isn’t going to remain in the lab or be treated as biohazards. Suits cover the scientists completely, including head and face coverings with fans that force air out as another level of protection against minuscule droplets of an aerosolized virus. Asked if he is anxious about working with serious and sometimes lethal viruses, Tarbet says he feels safer in the lab than in public where an aerosolized virus can be just another person’s cough or sneeze away.
Hurst is usually involved in training new employees and explained that after hours of required training, technicians gain experience with less dangerous viruses and only transition to BSL3 labs after they have demonstrated their understanding and willingness to follow all safety protocols. He says knowing he is working with a dangerous virus brings a heightened awareness to each procedure and he feels a responsibility to model safety because the longer people work in a lab, the more opportunities there are to become lax after a virus and protocols become familiar.
“Time goes more quickly in the BSL3 lab compared to outside the lab,” Hurst says. “Everything takes a bit more time to complete so I often find that I go into the lab for what I assume will be 45 minutes to an hour and then actually exit the lab two hours later. The other side of that is that the lab is very small and so incubation times can seem to slow down time when you are stuck in a small space for hours at a time. Either way, I usually end up at work much later than I plan to be here.”

Even in the midst of testing potential drugs to treat COVID-19, researcher Brett Hurst knows more viruses that threaten human life are coming. Photo by Levi Sim.
The current pandemic is just the most recent widespread case of a zoonotic virus, meaning one that moved from animals to humans. Others have made the jump from one species to another, including Ebola and West Nile viruses, and this iteration of the coronavirus will not be the last zoonotic disease to affect humans. Tarbet teaches a course in USU’s master of public health program on principles known as One Health—the concept that human, veterinary, and environmental health are inextricably connected and need to be studied and treated that way.
“We don’t have a miracle cure or way to prevent the spread of this virus, so we are doing the same things that we have done for months—social distancing, wearing masks, and increased hygiene procedures.” – Brett Hurst
“In the past 30 years, 70 percent of new and emerging diseases in humans have come from animals,” Tarbet says. “And 50 percent of physicians could not diagnose a zoonotic illness because it’s an animal disease. Human, animal, and environmental health are all part of one system and a change in one segment affects the others.”
Tarbet says changes in climate and the ways humans use land have complex and significant impacts on human health. The Centers for Disease Control and Prevention warn that climate change may increase the incidence of zoonotic disease outbreaks because climate directly impacts, among other things, where and how long a species can survive and spread a pathogen.
“It only requires a two-degree rise in global temperature and the species of mosquito that carries dengue fever could move into Minnesota,” Tarbet says. “And as things happen like forests burning in the Amazon and bulldozing into deserts, we destroy the wildlife space and bring ourselves closer to animals that harbor disease agents we haven’t seen in humans. We also eliminate species that may have served as buffers between us and viruses.”
When a new public health threat emerges, fear and prejudice often emerge emerge in the space between determining a disease’s origin and vector and discovering a treatment. Tarbet recounted traveling through part of New Mexico in 1993 and being astonished at a handwritten sign declaring “No Indians Allowed” on the door of a store. “I thought ‘Have I gone back in time? Is this the 1950s?’” Tarbet said. “But it was because of the hantavirus scare in the area. It was the first time we had seen hantavirus pulmonary syndrome.”
Later scientists pieced together that in the prior year there had been unusually high amounts of precipitation in the Four Corners area, which created an abundance of seeds and food for rodents, which increased the deer mouse population.
“So a desert mouse may have harbored that virus for millennia and had no problems with it,” Tarbet said. “But a new subdivision in the area was encroaching on desert land where people hadn’t lived before. So now people were sweeping out their new garages and kicking up dust with deer mouse fecal and urine material in it that contained hantavirus. They inhaled it and came down with a pulmonary syndrome that we had not seen before … People were scared and searching for the cause and their fear combined with ignorance and bigotry. It was not the Indians.”
One significant way SARS-CoV-2 is different from other viruses the IAR team has responded to is that so many people infected with the virus have no symptoms. Those asymptomatic carriers spread the virus because they often assumed they were fine, used few precautions, and amplified the curve we were supposed to be trying to flatten.
“We don’t know about asymptomatic carriers from other infections,” Tarbet says. “It’s possible we had them, but I don’t think we have ever seen that with the flu, for example. If you get the flu, you get sick.”
“People were scared and searching for the cause and their fear combined with ignorance and bigotry. It was not the Indians.” – Bart Tarbet
It’s also interesting that this virus largely does not cause disease in young people, though Hurst pointed out there have been cases of young, previously healthy people becoming quite ill with SARS-CoV-2. Just one more confounding aspect of this new disease.
“There may be something genetic involved in the ways people respond to the virus, but we’ll be figuring this out for a long time,” Hurst says. “I don’t see this going away soon even if we get a vaccine and better treatments.”
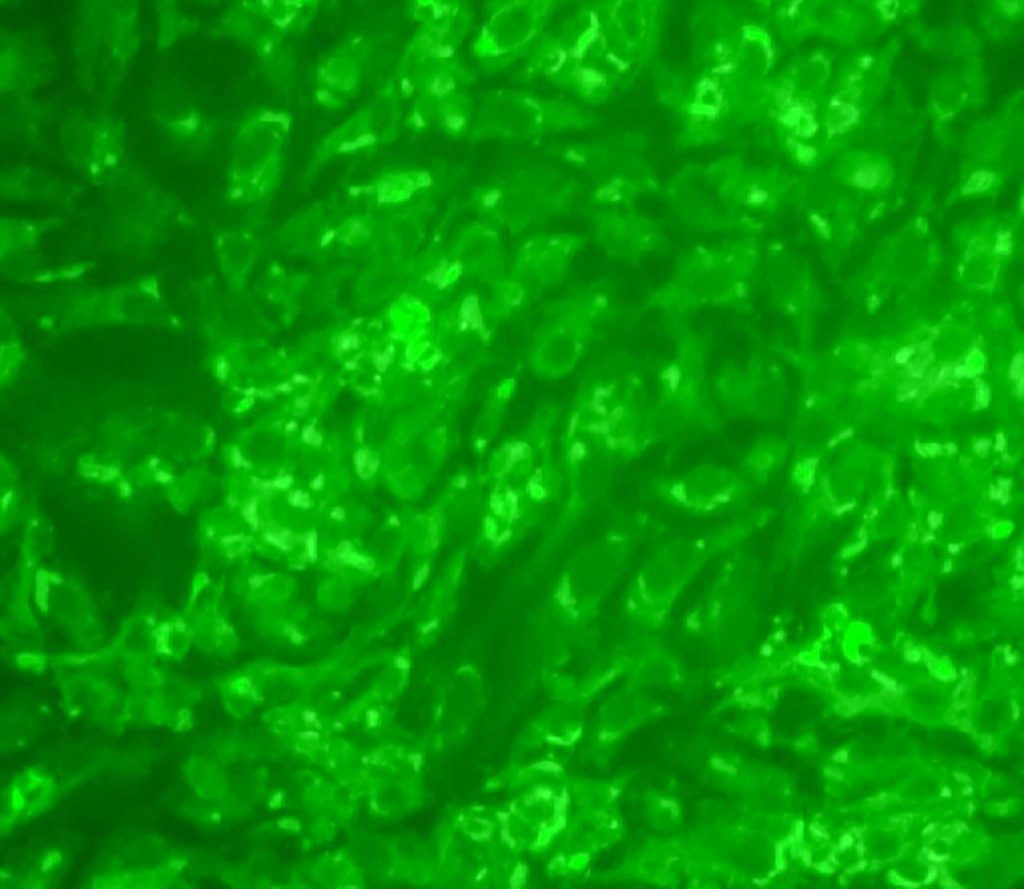
Ever wonder what the coronavirus looks like under a microscope? Image courtesy of USU’s Institute for Antiviral Research.
Tarbet added that even if a vaccine is tested and approved on an unusually rapid timetable, a significant percentage of the population won’t take the vaccine. One “social end” to the pandemic made numbers of SARS-CoV-2 cases in Utah and other states climb at record rates in mid-June, just as many cities and states were easing restrictions. The rising numbers weren’t all a result of more testing because percentages of positive tests and hospitalizations also rose. Graphing the numbers of cases and hospitalizations illustrated the problem even for those not fluent in math and statistics, but we can’t know for certain we are on the downhill side of the now familiar “curve” until we have passed the peak.
A major outbreak of an RNA virus wasn’t a surprise to scientists who are always watching for what the next one might be. When Zika made news in 2014 injuring and killing babies some wondered if that would be the next big outbreak.
“There has always been concern that we would have an outbreak like this one,” Hurst says. “But others have come and gone so when this coronavirus first hit we weren’t sure it was going to be the one. We just know that more viruses will always be coming.”
By Lynnette Harris ’88
Brett Hurst explains his work studying COVID-19, visit research.usu.edu/trainings-and-events/instead-podcast.