Youth Anxiety and What We Can Do About It
Two reports released by the Centers for Disease Control and Prevention this spring confirmed what many parents around the country have felt deep in their bones: kids are struggling.
The data indicates a youth mental health crisis preceded the COVID-19 pandemic and intensified during it. In late March, Debra Houry, the CDC’s acting principal deputy director, said the findings “echo a cry for help.”
In 2020, emergency room visits for mental health issues spiked by a quarter for children aged 5 to 11 and by nearly a third for youth 12 to 17. In 2021, 37% of high school students reported having poor mental health during the pandemic and 44% said they persistently felt sad or hopeless over the past year. This comes on the heels of an earlier analysis of national survey data collected from 2013 through 2019, which found that nearly 19% of high school students seriously considered attempting suicide.
These findings are bleak. And population level data can’t answer what is driving so many young people to despair. But embedded in the data are also kernels of hope. A factor called “school connectedness” seems to buffer the effect of the pandemic stressors. Individuals who felt connected to their peers and adults at school were significantly less likely to report feeling a persistent sense of sadness or hopelessness and less likely to consider and attempt suicide.
“Our research shows that surrounding youth with the proper support can reverse these trends and help our youth now, and in the future,” Houry said.
Changing the trajectory
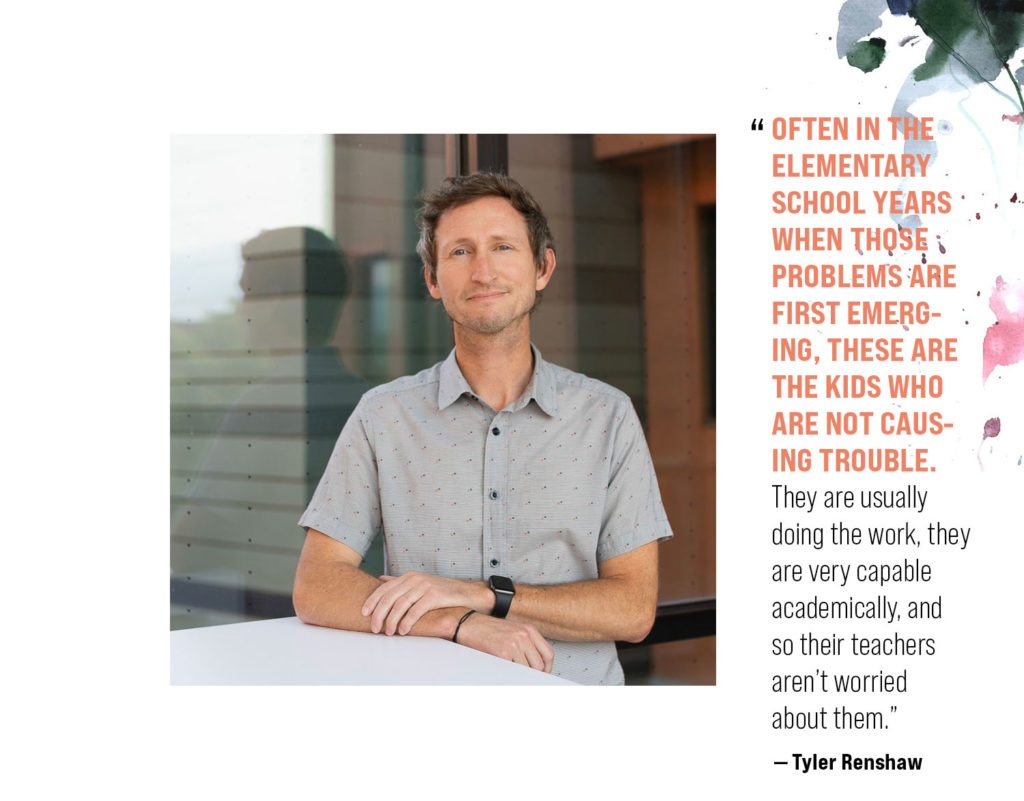
This squares with what Tyler Renshaw, associate professor of psychology at Utah State University, has seen from his research on school-based mental health services. When given the right behavioral and emotional support in school, it can change a student’s life.
“We have research that shows if you do very simple behavior management interventions with kids in kindergarten, by the time they become adults, compared to kids who didn’t get this intervention in their classroom, they are less likely to have contact with the juvenile justice system or to have substance use problems,” Renshaw says. “They are more likely to go to college. It really does increase the probability of future success in school, and their life, when they get these types of supports early on.”
That’s why, in 2018, when Renshaw started teaching at USU and learned that local schools didn’t have services in place to identify and help youth who may be at risk, he began calling administrators to see if they could use his lab’s services. Renshaw’s School Mental Health Lab provides both clinical counseling for secondary schools, as well as prevention efforts in elementary schools such as teaching self-regulation and problem-solving skills in classrooms and small groups so little issues don’t become big ones.
Because antisocial behavior — think bullying, aggressive behavior, or withdrawing from academic work — can start early and worsen over time if not stopped, Renshaw says.
His lab is now in its third year of partnering with Logan, Cache, and Rich school districts and has graduate student clinicians working with the various school counseling teams, which always seem to be overloaded with requests for help.
Traditionally, there are two pathways kids become candidates for mental health interventions in schools. One involves recommendations by teachers, caregivers, or peers. Typically, these are people who notice a change in a student’s behavior that is either harming to themselves or to others.
“It’s people seeing and hearing things that are very concerning,” Renshaw says, adding that other signs of a potential problems include truancy, academic failure, or not doing any work. “Kids basically have to be doing pretty bad and people notice.”
Universal screenings can flag the kids that fly under the radar, but who are struggling just the same.
Renshaw’s research specializes in universal school screenings that can help pinpoint classrooms and students in need of services by measuring indicators such as academic wellbeing and school engagement, and mental health concerns like anxiety, depression, conduct problems, and oppositional defiance. At the elementary level, teachers also fill out brief ratings of their students whereas in middle school and high school, students complete these questionnaires. Once scored, the data can be broken down to aid teachers in classrooms with more kids with elevated risk factors and potentially flag students who weren’t behaving in ways that raised any alarm bells.
“That’s why it is especially important that we do the screening for internalizing problems like anxiety and depression early on,” Renshaw says. “Because often in the elementary school years when those problems are first emerging, these are the kids who are not causing trouble. They are usually doing the work, they are very capable academically, and so their teachers aren’t worried about them.”
These screenings can identify those kids and connect them with services early on — either preventive or intensive if problems are more severe — so they don’t need individualized therapy later. Renshaw’s team leads group-based training with elementary students at risk for internalizing problems and teaches emotional coping and problem-solving skills so they don’t develop severe anxiety and mood disorders later, which typically worsen around adolescence, he explains.
And unless parents and caregivers are familiar with the signs of anxiety and depression in youth, they might miss them. Because they don’t necessarily manifest the way one might imagine.
“People think of anxiety as a kid who is cowering in a corner who is just afraid of everything,” Renshaw says. “Anxiety can be the kid who is throwing a tantrum when you are trying to drop him off at school, or it can be the teenager who is exhibiting severe aggression and cursing out their parents who are trying to force them go to church. Anxiety can also be the kid who is waking up every morning saying they can’t go to school because they feel sick because their stomach hurts or they have a headache, and they are not aggressive or mean, and they aren’t necessarily cowering.”
How did we get here?
Anxiety disorders among American youth are not new. But they have been slowly ticking upward over the years. Cell phones and social media are easy culprits to lay a portion of the blame, but even before students had the internet in their pockets, prevalence rates were already at concerning levels.
In the 1990s, some of our best estimates showed that 1 in 5 kids had what could be a diagnoseable health disorder, Renshaw says. As surveys contained more representative sampling that figure was adjusted to 1 in 6. One question that remains is why our kids are so anxious?
“We are always trying to get to the bottom of this, but we haven’t gotten to the bottom yet,” Renshaw admits. “We are getting better and better at gauging prevalence rates of mental health problems among youth.”
Anxiety and depression are often more likely to affect kids from minoritized racial and ethnic backgrounds and kids who are LGBTQ or identify with other marginalized groups. Conversely, these same groups are also less likely to get the support they need. There are considerable regional differences, too.
“Utah is in the highest quartile,” Renshaw says. “We have more kids with mental health disorders that are documented than do a lot of other states. You can see it like on a heat map like the prevalence of COVID.”
Utah is also in the highest quartile for lack of access to youth mental health services — a potentially dangerous combination. Schools are an appealing place to provide help at scale. They provide effective treatment and erase the traditional barriers that prevent adolescents from connecting with clinical care.
“It doesn’t matter how much money your family has,” Renshaw explains. “It doesn’t matter whether you have insurance or how good your insurance is, you get the services for free if they’re at school. It also doesn’t matter if your parents are working two jobs. It doesn’t matter if you have a car that can get you to the clinic. It doesn’t matter if there is another responsible adult in your life who can coordinate and schedule and do all of those things for you because most kids come to school most of the time.”
Having support services at schools not only makes mental health treatment more accessible to students, but equitable since they are connecting with individuals based on need rather than family resources.
Emerging treatments in schools

When COVID-19 hit, disrupting daily life across the globe, this pushed some individuals who were already struggling deeper into a hole. Therapists were booked solid and waitlists stretched for months. The need for services persists. Julie Petersen, a psychology doctoral student in USU’s ACT Research Group, works as a therapist on the Logan campus and witnessed the crunch firsthand.
“People are calling in every day,” she says. “Everybody, it seems, is looking for a therapist.”
Petersen studies treatment for obsessive-compulsive and anxiety disorders, particularly for youth, and specializes in Acceptance and Commitment Therapy (ACT) — a type of treatment that fuses mindfulness with action-oriented skills. The goal isn’t to change a patient’s thoughts and feelings — it’s to acknowledge them and function despite of them.
“ACT is a bit different from some other therapies that are more focused on changing challenging thoughts or feelings,” Petersen explains. “It’s more about changing your relationship with [them].”
For instance, she says, it’s being able to go to class even if there is anxiety, being able to play with your kids even if there is sadness.
Petersen recently conducted group therapy for high school students in Cache Valley as part of her master’s thesis. She wanted to test if ACT therapy, which is an effective treatment for stress, depression, and anxiety in adults, would be a useful tool for adolescents in schools.
The study, albeit small, was conducted with 26 students with elevated levels of anxiety who were randomly divided into either a school-based group ACT treatment or a waitlist for therapy. Individuals in the ACT group met one to two times a week for about an hour and practiced skills for making space for their anxiety and planning how to respond in various scenarios should it rear its head.
Petersen was surprised at the diverse identities of the kids who opted into the treatment, describing the group as having “a Breakfast Club vibe.” Afterward, the ACT group showed significantly less anxiety and class absences compared to the control group, providing evidence that ACT could be a promising treatment in schools.
“Utah State is the leading place to research these topics,” says Mike Twohig, professor of psychology and co-director of the ACT Research Group. “We were there when this work started and currently we are the ones doing the most work on this treatment.”
Their lab studies methods for teaching people how to be psychologically flexible other than just in one- on-one, in-person sessions, he says, adding that while that is useful, how do you get treatment to 100 or 1,000 people?
Petersen’s dissertation research involves examining the efficacy of individual ACT therapy delivered via Zoom for adolescents with health anxiety—a symptom that appears across a range of mental health problems that may manifest as a teen worrying they are sick with diseases like COVID or cancer, or obsessing about germs or handwashing. She is still recruiting participants for the study.
Back to baseline. Maybe.
In the early days of the pandemic, Mike Levin, professor of psychology and co-director of the ACT Research Group, saw an acute increase in seeking mental health services response among college students that eventually trailed off. And while he believes society, in general, is more aware of mental health issues and seeking treatment for them, he doesn’t see awareness as the driving factor pushing youth anxiety and depression rates upward.
“A chunk of what we are talking about, experiences of depression and anxiety, make sense in context often,” he explains. “We are beings navigating a world that can be really challenging and stressful and scary — socially, economically, in terms of basic safety, worries about health and unclear information about how to proceed. And all of those things should make us sad, they should make us anxious. Those are good natural responses that have a clear function.”
Feeling sad may indicate we are missing something in our life and feeling anxious may be alerting us to a threat, he says. Levin recommends listening to your internal world and using those feelings as a signal to “see what’s going on, make a plan.”
The problem is when people get stuck in those dark places.
“When you are really struggling to manage that pain, when you can’t do stuff in your life anymore, or you don’t know what to do with what you are experiencing,” Levin says, “I think that is when mental health resources can be really helpful for people.”
There is a theory called the hedonic treadmill, which suggests that people have an intrinsic baseline level of happiness. And after major life events — both positive and negative — those levels will fluctuate for a period and eventually return to baseline. That’s why the relative emotional high after getting married or winning the lottery fades over time as well as the heartache after someone we love dies.
It’s unclear if the spike in youth anxiety levels during COVID-19 are here to stay. Renshaw suspects the pandemic is a short-term huge stressor that worsened everything, but whose effects may disappear with enough time.
“We kind of assume the pandemic is like that but instead of being an individual kid or a family experiencing a traumatic event, it’s a population level experience,” he says. “But we expect that we will bounce back when we find a new normal.”
But we just need more distance — and data.
By Kristen Munson
Visit USU’s School Mental Health Lab or ACT Research Group for more information about services. Contact Julie Petersen at juliana.petersen@usu.edu if you are or have a student 12 to 17 who may be a candidate for ACT therapy for health anxiety.
Resources
Web-based free resources:
- Nemours Kids Health
- Child Mind Institute Family Resources Center
- CDC Children’s Mental Health
- Infoaboutkids.org
Evidence-based self-help resources online for adolescents:
- National Academies Wellbeing Tools
- Lab for Scalable Mental Health
- One Mind Psyberguide
- ACT Guide for Adolescents
Treatment finder:
Crisis support information:
- Call the National Suicide Prevention Lifeline @ 1-800-273-8255 (or use the online messaging and chat) for live support with suicide risk.
- For Utah residents, call the Utah Crisis Line @ 1-800-273-8255 to get live support with any kind of mental health crisis.
- For Utah students and educators, call the SafeUT Crisis Chat & Tip Line @ 833-372-3388 (or use the online messaging and chat) for live support during a crisis.